Vitamin D (Fourth Edition)
Chapter 57B - The IOM—Endocrine Society Controversy on Recommended Vitamin D Targets: In Support of the Endocrine Society Position
Vitamin D toxicity
Recommended supplement limits[edit]
The U.S National Academy of Medicine has established a Tolerable Upper Intake Level (UL) to protect against vitamin D toxicity ("The UL is not intended as a target intake; rather, the risk for harm begins to increase once intakes surpass this level.").[5] These levels in microgram (mcg or µg) and International Units (IU) for both males and females, by age, are:
(Conversion : 1 µg = 40 IU and 0.025 µg = 1 IU.[6])
- 0–6 months: 25 µg/d (1000 IU/d)
- 7–12 months: 38 µg/d (1500 IU/d)
- 1–3 years: 63 µg/d (2500 IU/d)
- 4–8 years:75 µg/d (3000 IU/d)
- 9+ years:100 µg/d (4000 IU/d)
- Pregnant and Lactating: 100 µg/d (4000 IU/d)
Acute overdose requires between 15,000 µg/d (600,000 IU per day) and 42,000 µg/d (1,680,000 IU per day) over a period of several days to months.
Suggested tolerable upper intake level[edit]
Based on risk assessment, a safe upper intake level of 250 µg (10,000 IU) per day in healthy adults has been suggested by non-government authors.[7][8]
The National Academy of Medicine, formerly the IOM, founded in 1970. has an excellent name, chosen to impress, but it has no more authority than its international competitor, the Endocrine Society, founded in 1916.
The NAM decided that the desirable level of vitamin D in blood serum should be at the observed average, which was 12ng/ml. Half of old folks in Baltimore were at less than 10ng/ml, while young people who go to the beach were much higher. while African shepherds are at 37-57 ng/ml.
At that point, smart doctors figured out that, to determine proper level for optimum health, we should not averages healthy and unhealthy bodies.
At that point, the NAM had to slightly bow to reality and revised its assessments in the direction of those of the Endocrine Society, although they covered up the earlier error by inventing the new category of insufficiency, to go between deficiency and sufficiency.
In 2011, Dr. Michael Holick, in the Journal of Investigative Medicine, published pages of impressive statistics:
“Lactating moms are at high risk for vitamin D deficiency even if they’re taking their prenatal vitamin. As a result they put their infant at risk for vitamin D deficiency if the infant receives as his or her sole source of nutrition human breast milk… For a lactating woman to put enough vitamin D in her milk to satisfy her infant’s requirement she would need to take 4000-6000 IU of vitamin D a day. Although this sounds like an extraordinarily high amount of vitamin D is very likely that our hunter gatherer forefathers exposed to sunlight daily were making thousands of IUs of vitamin D a day in their skin and therefore it is not unreasonable to believe that 4000-6000 IU of vitamin D a day is what we all require to satisfy our bodies’ requirement…
Infants who received 2000 IU of vitamin D daily during their first year of life were found 31 years later to have reduced their risk of developing type I diabetes by 88%… Women who had the highest intake of vitamin D were also found to reduce their risk of developing rheumatoid arthritis by 44%.(26)
It has been recognized for more than 20 years that living at higher latitudes increases risk of developing and dying of a variety of cancers including colorectal cancer, breast cancer, prostate cancer and pancreatic cancer. Women who had the most sun exposure as teenagers and young adults reduce their risk of developing breast cancer later in life by 50-60%. Women who had the highest intake of vitamin D reduce their risk of developing breast cancer by 50%. Postmenopausal women who took 1100 IU of vitamin D3 a day for four years reduce their risk of developing all cancers by 60%. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3738435/
It would appear that the NAM has slightly adjusted their judgement of appropriate D-levels, but their recommendations have not changed. They still preach fear of D, and recommend 600 IU.
The recommended dietary allowance is 15 µg/d (600 IU per day; 800 IU for those over 70 years). Overdose has been observed at 1,925 µg/d (77,000 IU per day).[citation needed]
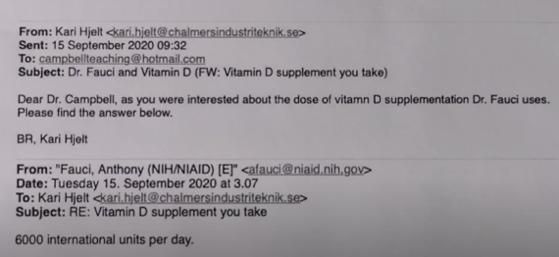
Important people, however, like Dr. Anthony Fauci, might take 6000 IU, but they mention it only to colleagues, they would not mention it to us ignorant masses who trust Wikipedia and the important people who set the rules.
Long-term effects of supplementary oral intake[edit]
Excessive exposure to sunlight poses no risk in vitamin D toxicity through overproduction of vitamin D precursor, cholecalciferol, regulating vitamin D production. During ultraviolet exposure, the concentration of vitamin D precursors produced in the skin reaches an equilibrium, and any further vitamin D that is produced is degraded.[9] This process is less efficient with increased melanin pigmentation in the skin. Endogenous production with full body exposure to sunlight is comparable to taking an oral dose between 250 µg and 625 µg (10,000 IU and 25,000 IU) per day.[9][10]
It has been questioned whether to ascribe a state of sub-optimal vitamin D status when the annual variation in ultraviolet will naturally produce a period of falling levels, and such a seasonal decline has been a part of Europeans' adaptive environment for 1000 generations.[12][13] Still more contentious is recommending supplementation when those supposedly in need of it are labeled healthy and serious doubts exist as to the long-term effect of attaining and maintaining serum 25(OH)D of at least 80nmol/L by supplementation.[14]
This editor really tries to say things unclearly. To make things a bit clearer, dark skin means that one is protected from sunburn, but may be 4 times less productive of vitamin D after an equal period of time in the sun. Result: very low vitamin D for Blacks in the U.S. Is it coincidence that Blacks suffer very high casualties from Covid-19? Some folks deny that, they may not like simple solutions and may prefer to ascribe the high casualties to "racism," which they have been promoting for a while as our major problem.
You'd think that non-racist wiki editors would explain the issue clearly: it may take four times longer for dark skinned folks to produce that vitamin D. Thus it would be very progressive to distribute vitamin D to the masses of all colours. However, the profit motive reigns supreme, and Big Pharma does not approve this kind of populism. So, no D for you!
Current theories of the mechanism behind vitamin D toxicity (starting at a plasmatic concentration of ≈750 nmol/L[15]) propose that:
- Intake of vitamin D raises calcitriol concentrations in the plasma and cell
- Intake of vitamin D raises plasma calcifediol concentrations which exceed the binding capacity of the DBP, and free calcifediol enters the cell
- Intake of vitamin D raises the concentration of vitamin D metabolites which exceed DBP binding capacity and free calcitriol enters the cell
All of these affect gene transcription and overwhelm the vitamin D signal transduction process, leading to vitamin D toxicity.[15]
Toxicity is easier to say than to observe. For years, millions of Americans have been taking vitamin D capsules without suffering any harm, except for a few cases of compulsive patients, who drank, every day, pharmacy-purchased vials of vitamin D, equivalent to a 100-capsule or 200-capsule bottle of 1000 IU. They did that, for months, before noticing that they were not feeling so well. The IOM-NAM mentions "risk of death" but does not mention lethal cases.
To find casualties, you need to cross the oceans. Occasionally, doctors make big mistakes, but even then there was not a big die-off of vitamin D extremists. For example, a one-year-old Italian child got 50,000 IU a day for three months. 32 cases of toxicity were observed in Kashmir, in patients aged 3 to 77 years, who had received injections of vitamin D between 1,800,000 and 30,000,000 IU. Of the 32 patients, one died, 4 were lost to follow-up, and 27 were declared cured.